Although microbiologically contaminated surfaces can serve as reservoirs of potential pathogens, these surfaces generally are not directly associated with transmission of infections to either staff or patients. The transferral of microorganisms from environmental surfaces to patients is largely via hand contact with the surface. Although hand hygiene is important to minimize the impact of this transfer, cleaning and disinfecting environmental surfaces as appropriate is fundamental in reducing their potential contribution to the incidence of healthcare-associated infections.
The principles of cleaning and disinfecting environmental surfaces take into account the intended use of the surface or item in patient care. CDC retains the Spaulding classification for medical and surgical instruments, which outlines three categories based on the potential for the instrument to transmit infection if the instrument is microbiologically contaminated before use. These categories are “critical,” “semicritical,” and “noncritical.” In 1991, CDC proposed an additional category designated “environmental surfaces” to Spaulding’s original classification to represent surfaces that generally do not come into direct contact with patients during care. Environmental surfaces carry the least risk of disease transmission and can be safely decontaminated using less rigorous methods than those used on medical instruments and devices. Environmental surfaces can be further divided into medical equipment surfaces (e.g., knobs or handles on hemodialysis machines, x-ray machines, instrument carts, and dental units) and housekeeping surfaces (e.g., floors, walls, and tabletops).
The following factors influence the choice of disinfection procedure for environmental surfaces:
a. the nature of the item to be disinfected,
b. the number of microorganisms present,
c. the innate resistance of those microorganisms to the inactivating effects of the germicide,
d. the amount of organic soil present,
e. the type and concentration of germicide used,
f. duration and temperature of germicide contact, and
g. if using a proprietary product, other specific indications and directions for use.
Cleaning is the necessary first step of any sterilization or disinfection process. Cleaning is a form of decontamination that renders the environmental surface safe to handle or use by removing organic matter, salts, and visible soils, all of which interfere with microbial inactivation.954–960 The physical action of scrubbing with detergents and surfactants and rinsing with water removes large numbers of microorganisms from surfaces.957 If the surface is not cleaned before the terminal reprocessing procedures are started, the success of the sterilization or disinfection process is compromised.
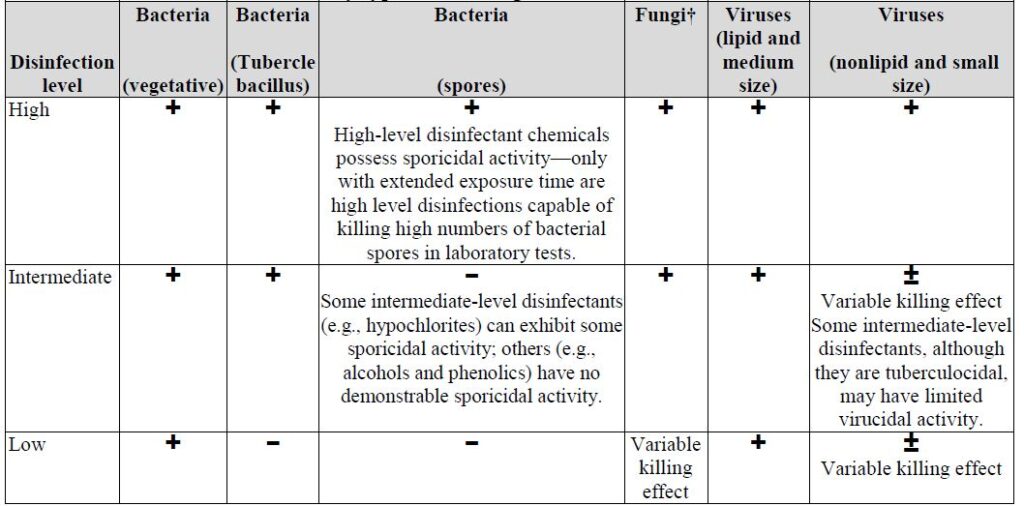
Spaulding proposed three levels of disinfection for the treatment of devices and surfaces that do not require sterility for safe use. These disinfection levels are “high-level,” “intermediate-level,” and “low level.” 949, 950
The basis for these levels is that microorganisms can usually be grouped according to their innate resistance to a spectrum of physical or chemical germicidal agents (Table 22). This information, coupled with the instrument/surface classification, determines the appropriate level of terminal disinfection for an instrument or surface.
Table 1. Levels of disinfection by type of microorganism
Refrences
Centers for Disease Control and Prevention (CDC)
Please Check out file at the following link
Heating, Ventilation, and Air Conditioning Systems in Health-Care Facilities
Modes of Transmission of Airborne Diseases
Environmental Infection Control in Health-Care Facilities
Disinfection in the Hemodialysis Unit
Transmissible Spongiform Encephalopathies in humans and in animals


