How does SARS-CoV-2, the virus that causes COVID-19, affect the human brain? Recent studies have given us clues, shedding light on why COVID-19 can be so severe for some people and why the symptoms can last a long time.
Those respiratory viruses included H1N1 and SARS-CoV. The SARS-CoV-2 virus, which causes COVID-19, is also known to impact the brain and nervous system.
Blood vessels scrutinized
Early in the pandemic, some infected people noticed a curious symptom: the loss of smell. Reports of other brain-related symptoms followed: headaches, confusion, hallucinations and delirium. Some infections were accompanied by depression, anxiety and sleep problems.
SARS-CoV-2 is known to penetrate the olfactory mucosa, causing loss of smell, and may enter the brain, migrating from the cribriform plate along the olfactory tract2 or through vagal or trigeminal pathways; however, definitive evidence for this is lacking.
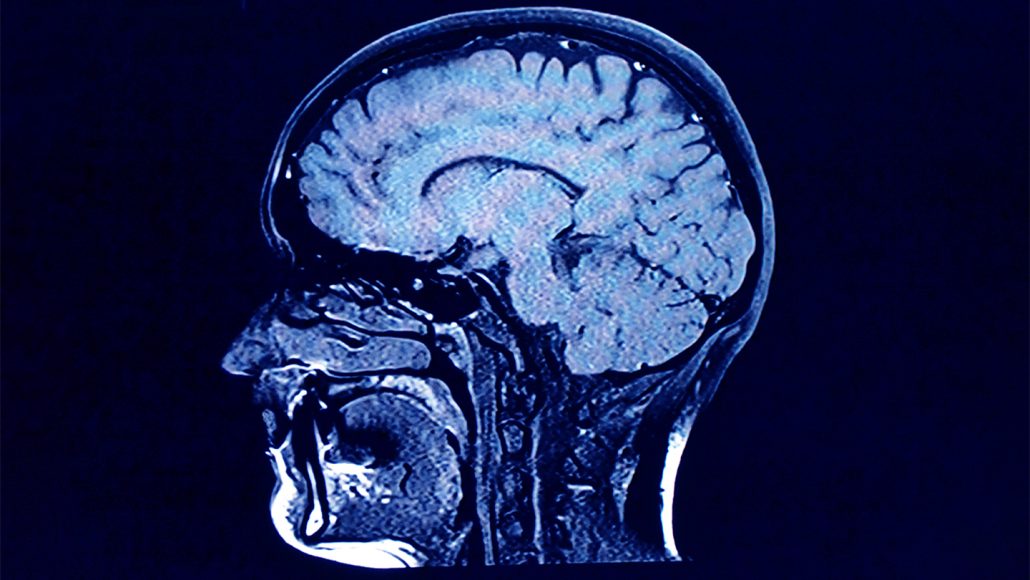
That absence suggests that the virus is affecting the brain in other ways, possibly involving blood vessels. So Nath and his team scanned blood vessels in post-mortem brains of people who had been infected with the virus with an MRI machine so powerful that it’s not approved for clinical use in living people. “We were able to look at the blood vessels in a way that nobody could,” he says.
Small clots sat in blood vessels. The walls of some vessels were unusually thick and inflamed. And blood was leaking out of the vessels into the surrounding brain tissue. You can see all three things happening at the same time.
Those results suggest that clots, inflamed linings and leaks in the barriers that normally keep blood and other harmful substances out of the brain may all contribute to COVID-related brain damage.
Inflamed body and brain
Inflammation in the body can cause trouble in the brain, too. Inflammatory signals released after injury can change the way the brain makes and uses chemical signaling molecules, called neurotransmitters, that help nerve cells communicate.
Patients with severe COVID-19 infection have been reported to experience a severe cytokine storm, with increased serum levels of proinflammatory cytokines including interleukin (IL) 1, IL-6, IL-10, and tumor necrosis factor (TNF)-α. TNF-α can directly cross the BBB by transport (increased BBB permeability due to cytokine-induced damage)4 or CVOs.
Some people with depression have high levels of inflammation, studies have found. We don’t actually know that that’s going on in COVID. We just know that COVID causes inflammation, and inflammation has the potential to disrupt neurotransmission, particularly in the case of depression.
For now, doctors are busy focusing on ways in which they can help, even amid these mysteries, and designing larger, longer studies to better understand the effects of the virus on the brain. That information will be key to helping people move forward. “This isn’t going to be over soon, unfortunately,” Troyer says.
It seems to be incredibly rare that you get viral central nervous system infection,” Michael says. That means many of the problems clinicians are seeing are probably a result of the body’s immune system fighting the virus.
Still, this might not be true in all cases, which means that researchers will need to identify biomarkers that can reliably distinguish between a viral brain infection and immune activity. That, for now, means more clinical research, post mortems and physiological studies.
Monday, May 3, 2021
Refrences
Please Check out file at the following link
COVID Antibody Responses and MS Patients
How long should sterilization monitoring records be maintained?